|
Donna Gregory Burch wrote an article entitled 13 Tips for Getting a Better Night’s Sleep with Fibromyalgia. This article is important to me, and I’m sure many of you, as many people with Fibromyalgia struggle with sleep. My sleep struggle has actually been present since I was very young; yet, others notice their quality and quantity of sleep decrease around the same time their Fibromyalgia symptoms begin to appear. I could write a book on disordered sleep and how to make your bedroom most conducive to sleeping. However, none of these things really help me as I still struggle to not only fall asleep but stay asleep. An important thing to note though is that although they may not work for me, it does not mean they won’t work for you. If you are struggling with sleep and you don’t have a regular bedtime routine and bedroom set up appropriately, that could be part of the problem. Ms. Burch, in her list of thirteen tips, talks about how to establish a bedtime routine and how your bedroom should be set up. I highly recommend that if you don’t have these two in place, that you follow her suggestions. They are spot on. If you follow these, and the other suggestions that Ms. Burch provides, I would request a sleep study. Having a sleep disorder IS common with fibromyalgia but they come in many forms and only a sleep study could determine what it is. If you’ve gone through all of Ms. Burch’s suggestions and are still struggling, let’s set up a time to chat. I have had to go through all of these plus more. I still struggle with sleep a lot (it’s probably what affects me most right now); but, I’m happy to offer suggestions and more helpful tips then what is offered here. Looking forward to hearing from you!
0 Comments
I’ve decided to tackle a topic that not many people want to talk about, but many people with the above diagnoses often experience. Before I get to the article, let me explain what the acronyms are for:
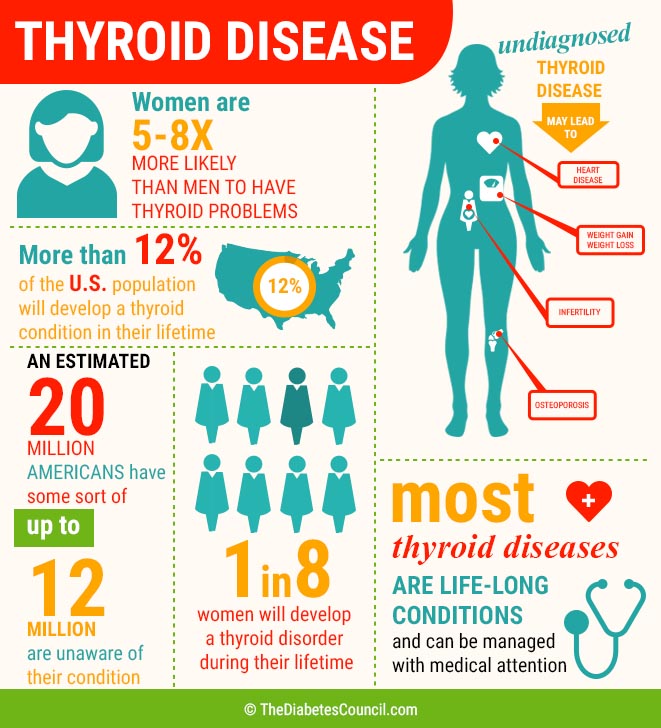
CFS = Chronic Fatigue Syndrome ME = Myalgic Encephalomyelitis SEID = Systemic Exertion Intolerance Disease. All of these are different terms for the same diagnosis. In the US, CFS is more commonly used and outside of the US, ME is more commonly used. I’m sure many more people are familiar with the acronym of IBS (Irritable Bowel Syndrome). According to the article, Irritable Bowel Syndrome in Fibromyalgia and CFS/ME, there is no known reason behind why these disorders/diseases are often connected; however, “we do know that all three conditions can include, imbalances of the chemical serotonin…” In my opinion, IBS is more easily treated that Fibromyalgia or CFS/ME, and it is important to treat the condition as IBS can cause the other orders to become inflamed. Talking about your digestive system is often not comfortable, but it is important to bring up your symptoms to your doctor so that they can be addressed. I struggled with IBS for many years, even before my Fibromyalgia and CFS diagnosis. While medicines worked a bit, changing my diet made a larger difference. If you would like some help to navigate this co-morbid diagnosis, OR need help with how to approach your doctor about it, I’d be happy to help! Six weeks into a new school year, at a new job, I quit. I was hurting physically and emotionally. My co-teacher was extremely verbally abusive towards me and in an 8AM-4PM day, she would only allow me to use the restroom once, and we didn’t get a break. We had to eat our lunch in the classroom and while she was allowed to be on her phone (using social media platforms and texting friends), I was not allowed to use mine. When we went outside, she and the other assistant would sit on a bench chatting away with their “favorite” child on their lap. They’d be on their phones, playing with the kids on their lap, paying no attention to the rest of the children in the class. We were in the infant room and were on a playground that was not developmentally appropriate for this age. Because the other two teachers sat on the bench, it was up to me to run around the playground making sure kids weren’t falling off playground equipment. There was one day where I was picking up a child to change his diaper, and noticed how much it hurt me. I made a comment about how it seemed more and more difficult to lift these children and the teacher said, “If you can’t lift these kids, this is clearly the wrong place for you.” Between that comment and all the other comments, she made me feel quite inept despite the fact that educationally and work wise I was more qualified than her. I quit. (This was after mentioning all this to the director of the preschool and getting no support.) As I looked back during those 6 weeks which were heavily peppered with Jewish holidays (so time off), I realized that I can home in tears and in pain every single day. I reflected back on a comment said in a group counseling session that I attended where, after describing my symptoms, people suggested that I might be struggling with fibromyalgia (something I hadn’t really heard about before), chronic fatigue syndrome, or another autoimmune disorder. I decided that since I was no longer working, while looking for a job, I would connect with my doctors to see if I did indeed have one of these disorders. The doctor I was seeing at the time was at a sliding fee scale clinic as I did not have health insurance during the time (I was denied due to a pre-existing condition of asthma!!). As I brought up fibromyalgia to this doctor, she threw her head back and laughed saying, “you don’t have fibromyalgia. It’s not even a real thing. It’s an exclusionary disorder at best. You’re struggling with severe depression which can cause pain in people.” Who was I to go against someone who had spent so many years in medical school and as a practicing doctor? Thankfully, not long after, I was able to get insurance and switched to another doctor. Long story short (as you know I am good at the long stories), I brought up fibromyalgia to the PA I was seeing there. She didn’t deny my thoughts but suggested we do a full blood panel to eliminate any other disorders or diseases that may explain my symptoms. When that panel came back clear, I asked if I could now see a specialist that works with people with fibromyalgia. She agreed to refer me to a rheumatologist. I’m going to stop there. I know how hard it is for many of us to focus so this will be a multi-part series on my journey. If you identify with some of this, or are considering application to disability, please feel free to reach out and I can help you with the knowledge that I now have of the experience. Did you know that thyroid disorders are often misdiagnosed as fibromyalgia? Did you also know that you can have normal TSH (Thyroid Stimulating Hormone) levels and still have a thyroid condition? The protocol for assessing someone as to whether they have fibromyalgia is generally to rule out other conditions, especially autoimmune conditions, before making a diagnosis. Donna Gregory Burch authored an article entitled The Fibromyalgia-Thyroid Connection. If your TSH thyroid test is normal, you better read this… stating that the TSH test alone is a poor indicator of whether or not you have a thyroid disease. Since my teens, I have been displaying symptoms of hypothyroidism (my mom has Hashimoto’s disease) but my thyroid tests have always come back “normal.” It wasn’t until I saw a naturopath who concluded that my thyroid was overworked and needed to be treated, so she sent me to a doctor (my current primary care doctor) who also agreed that I needed treatment. I was put on a low dose of synthroid and it made a huge difference in my fatigue and energy levels. As my body became accustomed to the medicine, I felt better almost instantly. Ms. Burch interviewed Dr. David Brady, a fibromyalgia specialist about why thyroid dysfunction was overlooked when assessing for a fibromyalgia diagnosis. Dr. Brady commented on the fact that it is possible that one can be diagnosed with both conditions and while they have similar symptoms, they need to be treated rather differently. In order to evaluate whether one has thyroid disease, Dr. Brady “order[s] a TSH. [He also] order[s] a total T4, a free T4, a total T3, a free T3, and then particularly if there’s any family history of Hashimoto’s, Grave’s or any type of autoimmune thyroid condition, we order what are called TPO antibody and thyroglobulin antibody [tests].” You can find out more about what T4 and T3 are in the article. If you have been diagnosed with fibromyalgia and are still experiencing fogginess, fatigue, exercise intolerance, muscle aches, thinning hair and more, I would recommend getting your thyroid function testing done. In the article, Dr. Brady suggests that thyroid testing should be done either by a functional medicine or integrative medicine doctor. There is a significant amount of important information in this article as well as many wonderful suggestions. I highly suggest you read the article alongside my very condensed summary. With lessons from my own fibromyalgia and thyroid diagnosis journey, I’d be happy to help you with yours and get you to a place where you are feeling better. In my coaching course and research of my own, I will gladly help you understand more specifics of thyroid disease as well as help you find a doctor in your area that will do a full thyroid panel. Like I stated above, fibromyalgia and thyroid disease (especially hypothyroidism) have a lot of overlapping symptoms. Don’t let your thyroid go untreated by attributing all of the symptoms to your fibro! Looking forward to helping you out in any way I can! Faith is another one of those difficult to approach topics. When I refer to faith in this blog, I refer to religion. Specifically, I am referring to faith in G-d. In a 2016 study presented by Gallup.com 89% of people polled in the United States believe in G-d or a “universal spirit.”
Then when you are diagnosed with a chronic condition or scary illness, faith can waver. I’m someone who strongly believes in G-d, yet, there were many times I was angry with G-d for the major life changes that chronic pain and autoimmune disorders cause. I’m sure many of you can identify with this situation. Right now, G-d and I are on pretty decent terms and we have open communication, so things for me in that department are all good. In an article entitled “Illness Doesn’t Equal Lack of Faith,” Suzanne Stewart, the author discusses that people that may be overzealous or “fundamentalists” (her quotations, not mine) will blame your diagnosis on your lack of faith in G-d, or a higher power. I can identify with this. I was once told, by an observant friend (I wasn’t as observant at the time), that life threatening illnesses are caused by your lack of faith in G-d. I was shocked. I had never heard such a thing. A few years later, I had moved away for graduate school and received a call from this friend. She called to let me know that her father passed away from a brief but terrible illness. My mind started racing. Despite this comment that my friend made, her family was kind, wonderful, and giving. They invited me for Sabbath and holy day meals all the time. Her father radiated nothing but kindness and now he was dead. I, of course, never mentioned what my friend had said in connection with her father, but I knew it couldn’t be true. I’ve also been sent messages, since I’ve started blogging and posting articles on my Facebook page that I’m ill because I don’t accept Jesus as my savior. If you haven’t figured it out yet, I’m Jewish. At first I was angry at these people, but then realized it was a level of ignorance surrounding my faith. And, ignorance comes out strong with illness. I believe these people meant well, but their knowledge, biblical or otherwise was sorely lacking. Stewart ends her article with the following statement: “I’m not here to judge any of these Faiths or beliefs, but I am here to say that nobody is sick because of their belief system or lack of faith. People don’t live with chronic pain day in and day out due to any Religious affiliations or lack thereof. We don’t use a cane, a wheelchair or a walker because we do not pray enough. It does not help a person with chronic pain and illness, to approach them and say any of the words that I’ve stated above. If you choose to pray for someone, then you can do that. But don’t try to push guilt and more pain onto anyone who’s already suffering. That doesn’t help, it only hurts and makes things much worse. Please try to remember to treat others as you would wish to be treated.” We need to take this information to heart. As much as it feels like a punishment to have Fibromyalgia or any other chronic pain or autoimmune conditions, no one, including G-d, is punishing us. It took me a long time to recognize this, but my diagnosis lead me towards wonderful things including becoming a Fibromyalgia Advisor as well as making incredible friends who just happen to share the same disorder. We also need to share this information with those who are giving unsolicited advice. Share this article with someone who might be doing this, and they may learn something from it. I am very connected to my faith, but I don’t push it on anyone. If any of you are interested in learning how your faith can help you get through some of the tougher times with chronic illness, please free to drop me a line. I’m looking forward to hearing from you soon! Another Jewish holiday happened about two months ago (Yes; another holiday. We have many them!). This holiday is called Shavuot. The word Shavuot actually means “weeks.” The holiday commemorates the date that G-d gave the Torah (Old Testament to those of you who don’t know the Hebrew term) to the Jewish people at Mt. Sinai over 3,300 years ago. From the beginning of Passover to Shavuot, we count 49 days, the amount of time it took Moses and the Jews to reach Mt. Sinai to receive the Torah. We celebrate this holiday by lighting candles, staying up all night to learn Torah, hear the reading of the Ten Commandments, and many have the tradition of eating dairy foods. Why am I telling you about this holiday? Because I feel like, with all the other Jewish holidays, there are applicable lessons we can learn with regard to how we manage our Fibromyalgia.
What could be learned from getting the Ten Commandments? Well first of all, we can apply some of the commandments to how we live our life with Fibromyalgia. I read an article by Chana Weisberg entitled "10 Bite Sized Life Lessons to Be Learned from the 10 Commandments." While not all the lessons listed apply to us Fibromites, I thought I could take a few of her lessons and guide you towards a more meaningful life while living with a chronic pain disorder. 1. “G-d chose to give the Torah on an elevated mountain. You can elevate your life.” As we know, a diagnosis and life lived with Fibromyalgia can be upsetting, depressing, frustrating, and the like. However, it doesn’t have to be. I can’t speak for everyone else but I believe I was chosen by G-d to have this disorder (as annoying and frustrating it is sometimes) to get me to follow my life’s path. I believe that becoming a Certfied Fibromyalgia Advisor was what I was meant to be and all my previous jobs were steps toward this ultimate goal. How does this apply to you? Well, no one wants to think G-d gave them something that could be potentially awful and life altering, but I have found with my clients, together we can find something positive about having this disorder. One thing that I can think of that everyone can do to elevate your life with Fibromyalgia is to EDUCATE. Fibromyalgia is still often thought of as a “wastebasket disorder/diagnosis” by many in the medical field, and therefore anyone else who does not live with this disorder. We can take it upon ourselves to help others, INCLUDING medical professionals, so that we can be taken seriously. Having done this myself, I don’t feel like I struggle with the disorder as much as I did before - when everyone thought my diagnosis was all in my head! 2. “A mountain is the same dirt as a plain, but has been raised. No matter how dirty your life appears, raise it and make of it a mountain.” People are going to judge you. You might even judge yourself, but, as with the lesson above, you have the option to change how people view and think about you, and how you think about yourself. You may feel with this diagnosis that you’ll never do anything again; however, YOU CAN and by doing so, you can show others that while your life has changed, you won’t let Fibromyalgia stop you. So, not only do you need to protect yourself from others, you also need to protect yourself from your own thoughts and feelings about how this disorder is affecting you. Being diagnosed with Fibromyalgia or living with it for many years can make you feel more like a “dirty plain.” But, if you treat yourself they way you deserve or realize you can live a full life with fibro, life goes on and you've turned your “dirt” into a mountain and have most likely elevated the way you feel about yourself, therefore not allowing your diagnosis to take over your life. 3. “The 10 Commandments were addressed in the singular form to the whole of the Jewish people; if even one Jew was missing, the Torah could not have been given. You are essential. Hmmm... How can Kate apply this to living with Fibromyalgia? Challenge accepted! I’m taking one small segment from this lesson to show you how the whole piece applies. You are essential. This is a struggle many people with fibromyalgia to deal with as they try to figure out how they can contribute to the community, their family, and themselves. Fibromyalgia certainly changes one’s life, however, you can still live a happy and full life. It just may not be the one you were expecting/planning. As they say, “Man plans; G-d laughs.” I’m sure a good deal of might take offense to this statement ( I do too, sometimes.), but, I truly believe G-d has a plan for you, and while it may not be what you planned or expected, G-d still believes you are essential to this world. This is where we can connect the “singular form” to the whole. You are one single person. How much can you do? So much! We often feel we lose value because our pain and fatigue doesn't allow us to participate in as many things that used to be so simple like daily chores, or cooking dinner; but, it's important for you to know that you are valuable just because you are you. It's also important to note that just because you have Fibromyalgia, having the disorder doesn't make you any less valuable! In my case, I went from being an educator, to feeling like life had nothing left to give me (after the Fibromyalgia diagnosis), to coaching others with Fibromyalgia, other chronic pain disorders and their co-morbid diagnoses. Coaching has given me life and purpose in a way that I didn’t think anything could aside from working in the field of education. Coaching is obviously not for everyone; however, even with your diagnosis, there is still so much that you can offer to this world. Need some help with that? That’s where a coach can come in. ;-) 4. “The Ten Commandments were said to individuals, tailored to each person’s spirituality and psychological makeup. You have a unique role and mission.” This piggy-backs on the previous one. Again, it’s important to realize you haven’t lost yourself nor your identity due to the Fibromyalgia diagnosis. Things DEFINITELY change, often times your whole life is flipped upside down, but it’s your decision and your mission to figure out how to live life with this new “makeup.” Fibromyalgia is a hard diagnosis to swallow. Allow yourself to mourn, be sad, and be upset. But, don’t allow yourself to decide that life is over due to the diagnosis, because it’s not. You still have much to offer and sometimes it takes some time to figure out what that is. Only you know your abilities and limitations, so only you can make the decision about your next step in life. 5. “The Jewish people were ‘facing the mountain’ ready to receive G-d’s word. If you focus on something higher, petty differences disintegrate.” I’ll admit it, Fibromyalgia is a challenge. And, I’ll admit many of us try to focus on achieving the larger goal. I have learned, sometimes painfully, that to “survive” with Fibromyalgia, you need to cut these larger goals into tiny baby steps because if you try to do the whole goal all at once, it may never be attainable. Petty differences can get in the way of your goal(s). (Unfortunately) Life changes happen when you are diagnosed with Fibromyalgia. I discussed this above. You make the decision as to whether this will affect you negatively or positively (hopefully the latter). If you continue in your path of how horrible this diagnosis is and that you’ll never lead a “normal” life again, “petty differences” certainly get in the way as you are focusing on barriers that can never be attained as opposed to obstacles that can be overcome. As hard as it is, let go of these “petty differences” so that you can climb those mountains, jump over those hurdles, and live a happy and full life while living with a chronic pain disorder. Sometimes being able to switch your thinking from barriers to obstacles can be difficult, especially early on in your diagnosis. However, having someone to help you through these hurdles will make the transition much easier. A Fibromyalgia coach/advisor, who may have dealt with the same hurdles you have, can help. We can share with you what might have worked for us and/or things that have worked for friends or fellow coaches. Additional Thoughts For those of you that believe in G-d, or feel connected to a higher power through spirituality, you may believe, alongside myself and my fellow coaches and advisors, that having a coach is beneficial, and (I can only speak for myself here) crucial for my ability to function while living with chronic illness. Many of the “larger” religions believe in Ten Commandments and are required to live by them. And, as I discussed above, you can apply the lessons you learned from them to your daily live of living with a chronic illness like Fibromyalgia. Are there any lessons you have applied to the way you have chosen to live your life that can be gleaned from the Ten Commandments? If so, I’d love to hear what you’ve learned. I want to express that I have my own coach and working with her has been life changing. She has helped me view life through the eyes of a Fibro Warrior in a different, more positive way. I have learned that challenges can be positive and can support our struggles in a big way. I don’t think I would feel as well (physically or emotionally) without having a coach (and friends that are coaches) to help me through the transition of living with a chronic illness. Need some help with re-connecting to your faith that you might have lost after your diagnosis, or just help with “surviving life” with Fibromyalgia? Reach out to me or another coach to get some support. I offer a complimentary consultation with no commitment to continue to help you decide if coaching is for you. We can often schedule something within a week’s time. (If you click on the word schedule, it will take you directly to my scheduling page.) In the meantime, I hope something in this blog post resonated with you. There will be more to come. My goal is to help as many people living with a Fibromyalgia diagnosis, their co-morbid diagnoses, or any other chronic pain sufferers as I can. I look forward to hearing from you soon! =) Several weeks ago, I was chatting with a fellow Fibro Warrior of mine and somehow we got onto the topic of whether fibromyalgia was progressive. My thoughts, from some research and my own experience with the disorder, was that NO; it was not a progressive disorder. My friend, who has lived with the disorder over 20 years against my almost five years, politely disagreed stating that she felt her observations led her to believe that YES, fibromyalgia IS a progressive disorder. In this article, http://fedupwithfatigue.com/is-fibromyalgia-progressive, many doctors weigh in and share their opinions on observations and research. I will explain after I summarize the article why I believe fibromyalgia is not a progressive disorder. First, it’s important to address the definition of progression. According to Dr. Ginevra Liptan of the Frieda Center in Portland, Oregon: “what physicians mean by ‘progressive’ illness is one which function is lost over time...multiple sclerosis, an illness characterized by progressive nerve damage and loss of muscle function.” According to most doctors interviewed in the article, the disorder of fibromyalgia itself is not progressive. However, there are symptoms that if are not treated correctly (i.e. under a doctor’s care is one example), can become progressive because they aren’t being addressed. Many compare the situation to exercise. If a doctor recommends exercise or physical therapy for a broken leg, physical therapy helps the muscles that had not been used for weeks or months to keep from atrophying. An example connected to fibromyalgia is the struggle to have restorative sleep. If you cannot address and find a way to address this issue, your pain and fatigue is likely to increase. Doctors Randall Gates and Martin Rutherford, who run the Power Health Rehab and Wellness Center in Reno, Nevada state that “...the graduate decline seen with fibromyalgia is due to the chronic, autoimmune and or degenerative nature of the underlying causes associated with the condition.” Two of the doctors disagree with the majority consensus stating that there IS progressive degeneration from Fibromyalgia. Dr. Neil Nathan from the Redwood Valley Clinic in Redwood Valley, California, and Dr. Richard Podell of the Podell Medical Practice in Somerset, New Jersey both agree for some people, fibromyalgia can be degenerative. While they are in the minority, they backup their comments. However, in a similar fashion to the doctors who don’t believe it is progressive, these doctors state it is likely the co-existing conditions that often come along with fibromyalgia that make it appear progressive. The example they both use is Chronic Lyme disease which CAN do irreversible damage to your body. The interesting thing is those that are stating that fibromyalgia is progressive are still stating it’s due to their co-morbid diagnoses and therefore, in my opinion, make their argument weak. In going back to the discussion with my friend, she does have many coexisting diagnoses and agreed they could be making her fibromyalgia worse, however, she still believes her fibromyalgia has gotten worse over time. I guess I’ve been lucky and have found the combinations of medications, therapies, and supplements that make me think fibromyalgia itself is not a progressive disorder. However, since my diagnosis, I have received a couple of co morbid (common) diagnoses that do often make it feel as though maybe my fibromyalgia has gotten worse; yet, I need to remember and remind myself that my coexisting diagnoses, while having overlapping symptoms with fibromyalgia, are an entity of their own and it is possible that the symptoms of THOSE disorders and diseases are worsening, and it is separate from the fibromyalgia. How do I justify this? When I started to get new symptoms after my fibromyalgia diagnosis, I just attributed it to the fibromyalgia. However, after connecting to an incredible naturopath and primary care doctor (who also has fibromyalgia), as well as taking the coaching course, I have learned a new symptom need not mean fibromyalgia. I’ve learned to talk to my medical support team and that’s been helpful. So, after reading my not so short synopsis, you can see why I’ve come to my conclusions. However, I am sure there are other patients and doctors who think otherwise. I’d love your input, your thoughts and feelings about the issue. Do you think fibromyalgia is progressive? Why or why not? If you do, how do you rationalize your decision? |
AuthorI’m Kate Straus and I’m a Certified Fibromyalgia Advisor. I help Jewish women feel confident in their ability to practice their faith while navigating the ups and downs of fibromyalgia. I’m using the disease that at one time knocked me down, to help support others live life to their fullest. Archives
January 2021
Categories |





 RSS Feed
RSS Feed


